Advanced degenerative disc disease treatment in Atlanta
Motion-preserving disc care with artificial disc replacement, facet stabilization, and customized rehab to protect long-term spinal health.

Your discs are wearing out, but your life isn't over. Degenerative disc disease might sound scary, but it's actually a natural part of aging—the key is how we treat it. At Legacy Brain and Spine, we're national leaders in motion-preserving solutions that traditional spine surgeons often overlook. While others rush to spinal fusion (which limits movement), we specialize in lumbar artificial disc replacement—a revolutionary approach that relieves pain while maintaining your spine's natural motion. Stay active, stay mobile, stay you. That's our promise.
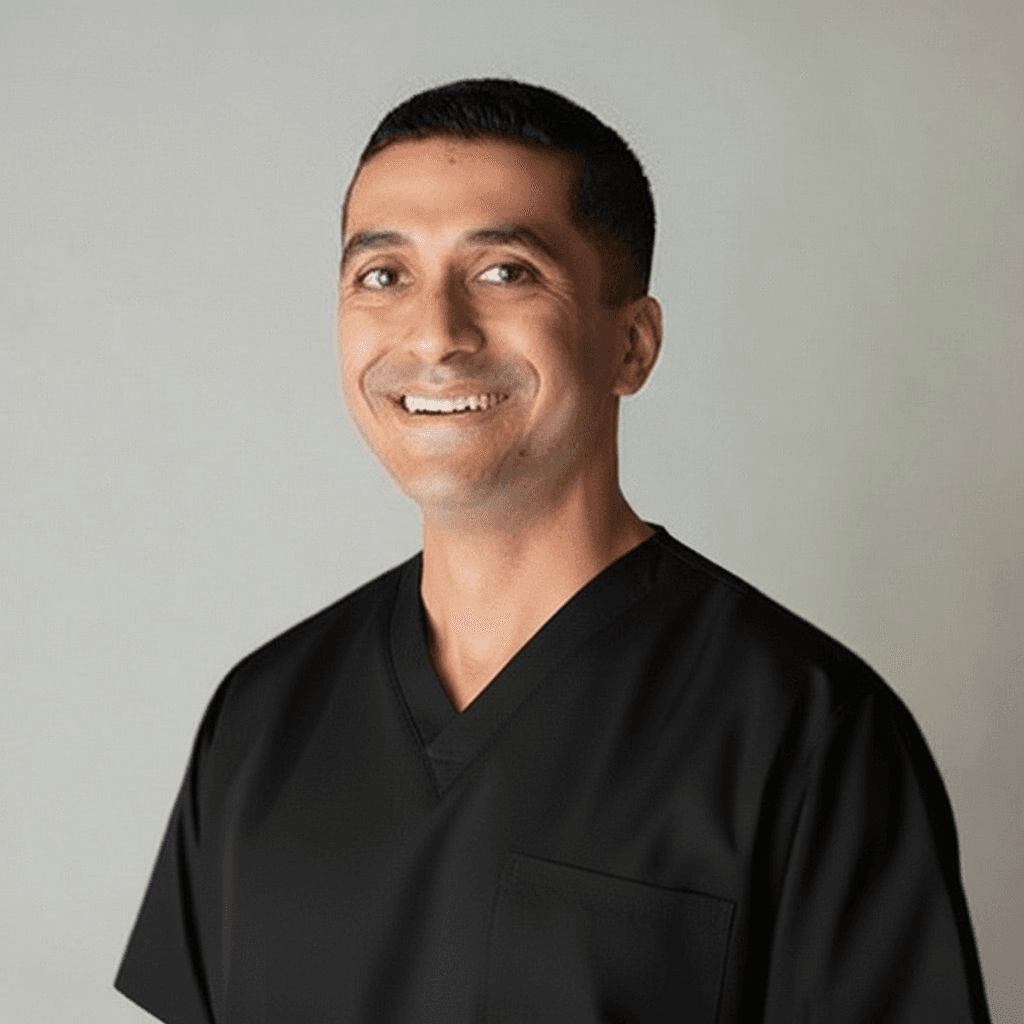
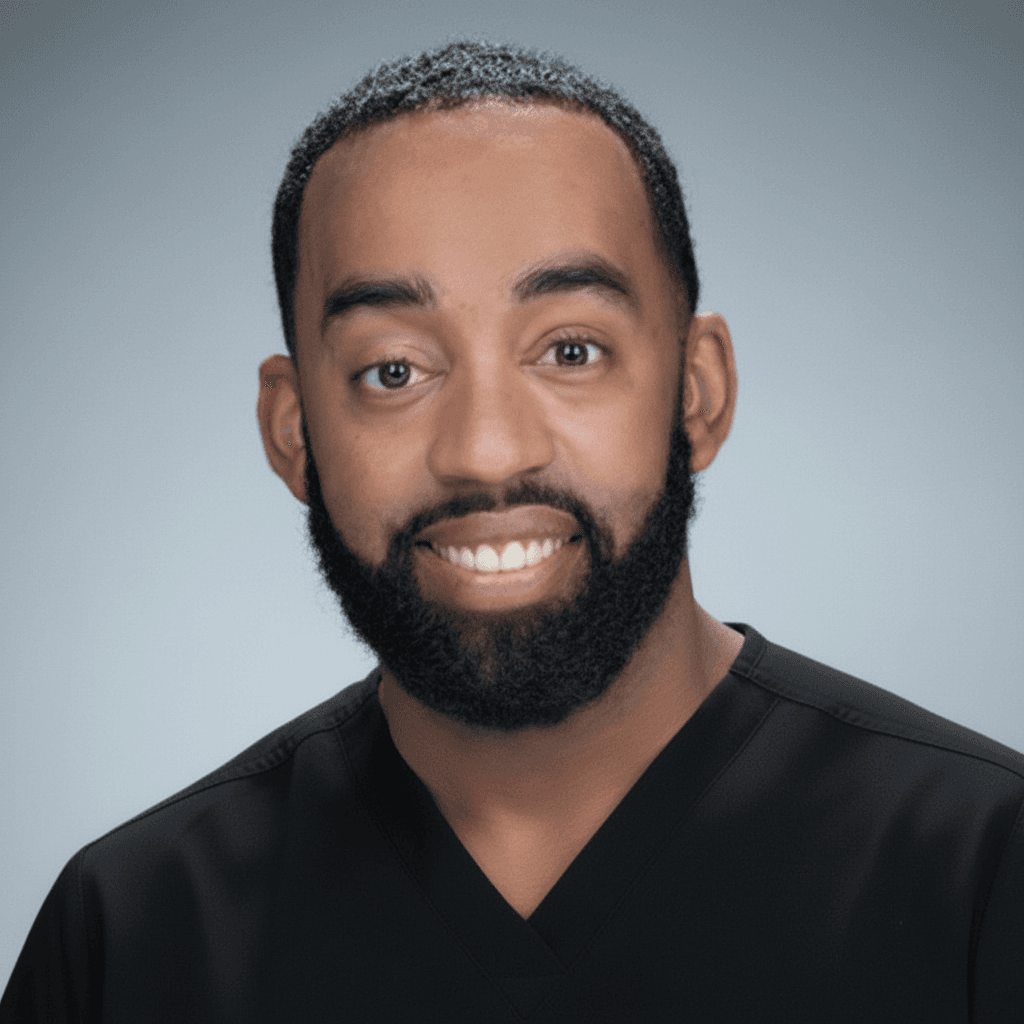
Our Specialists
Meet the physicians who specialize in treating degenerative disc disease:
Available at these Locations
This treatment is available at all of our convenient locations:
Overview
Degenerative disc disease is not actually a disease but rather a condition where natural age-related wear causes pain. As discs lose hydration and height, they can cause pain and other symptoms. Legacy specializes in motion-preserving alternatives including artificial disc replacement.

Expert care for degenerative disc disease
National leaders in motion-preserving lumbar disc replacement offering alternatives to traditional fusion. Our expertise in artificial disc replacement provides lasting relief while maintaining spinal mobility and rapid return to activities.
Common Symptoms
Discogenic pain—pain originating from the disc itself—has characteristic features. Unlike nerve pain that shoots down the leg, disc pain typically remains in the back, worsens with sitting and bending, and improves with position changes. These flare-ups can be unpredictable and debilitating. Understanding this pattern helps confirm the disc as the pain source and guides treatment toward disc-specific solutions rather than nerve treatments.
Chronic low back pain
Persistent discomfort lasting months or years with fluctuating intensity, creating constant background pain punctuated by acute flares. This ongoing pain stems from the degenerating disc itself rather than nerve compression, significantly impacting daily function and mood.
Pain worsens with sitting or bending
Forward-bending activities and prolonged sitting dramatically increase disc pressure, intensifying pain. Desk work, driving, or sitting through meals becomes progressively more difficult as the day wears on and disc stress accumulates.
Pain improves with walking or position changes
Movement and upright walking actually feels better than static sitting because it varies disc loading and promotes fluid exchange. Many patients report relief from short walks but return of pain once sitting resumes.
Intermittent severe episodes
Chronic baseline pain is interrupted by acute flare-ups of severe, debilitating pain triggered by specific movements, overactivity, or sometimes no identifiable cause. These episodes can last days to weeks, requiring rest and escalated treatment.
Pain radiating to buttocks or thighs
Referred pain extends into the buttocks and upper thighs without following a specific nerve pattern. This discogenic pain differs from true sciatica but indicates significant disc disruption with inflammatory mediators irritating nearby structures.
Weakness or numbness if nerve affected
When degenerative changes progress to nerve compression, new symptoms of numbness, tingling, or leg weakness emerge. This evolution from discogenic to radicular pain signals more advanced disease requiring different treatment considerations.
Common Causes
While disc degeneration affects everyone eventually, not everyone develops painful symptoms. The difference lies in how dramatically discs degenerate and whether they develop tears that expose pain-sensitive nerve endings. Genetic factors, previous injuries, smoking, and occupational stress all influence who develops symptomatic degeneration. Understanding your specific risk profile helps prevent progression and guides treatment toward motion-preserving solutions.
Natural aging process
Everyone's spinal discs naturally dehydrate and lose elasticity over time, starting in our 30s. This universal aging process causes discs to flatten and become less effective shock absorbers, though not everyone develops painful symptoms from these changes.
Loss of disc hydration
Discs contain mostly water when we're young, but gradually lose fluid content with age. This dehydration makes discs less flexible and more prone to tearing, reducing their ability to cushion vertebrae during movement and bearing weight.
Tears in disc outer layer
The tough outer ring of the disc (annulus fibrosus) develops small tears from repetitive stress or injury. These tears allow the gel-like center to leak out, causing pain both from the disc damage and from inflammatory chemicals irritating nearby nerves.
Previous injuries
Past trauma from accidents, falls, or sports injuries can initiate disc degeneration earlier than natural aging would cause. Even injuries that seemed minor at the time can start a degenerative cascade that progresses over years or decades.
Genetic predisposition
Research shows that genetics play a significant role in disc health, with some families experiencing accelerated degeneration. If your parents or siblings have disc problems, you're at higher risk for developing degenerative disc disease at younger ages.
Treatment Options
Physical therapy and exercise programs - Structured program emphasizing core stability, flexibility, and low-impact aerobic conditioning to support degenerating discs
Anti-inflammatory medications - NSAIDs and other medications to manage inflammatory pain while pursuing other treatment modalities
Lifestyle modifications - Weight management, smoking cessation, ergonomic improvements, and activity modifications to reduce disc stress and pain
Lumbar artificial disc replacement - Revolutionary motion-preserving surgery replacing worn disc with flexible artificial implant, maintaining natural spine movement unlike fusion
Spinal fusion for severe cases - Surgical joining of vertebrae to eliminate painful motion when disc replacement isn't appropriate or other treatments have failed
Regenerative medicine options - Emerging treatments like platelet-rich plasma (PRP) injections to potentially stimulate disc healing and reduce degeneration
State of the art facilities
Joint Commission Gold Seal certified surgery centers equipped with the latest neurosurgical technology. Our Atlanta and Riverdale facilities offer minimally invasive procedures with concierge recovery suites for optimal patient comfort.
Recovery & Outlook
Motion-preserving disc replacement typically allows return to activities in 6-12 weeks. Our surgeons are national leaders in multi-level disc replacement, offering alternatives to traditional fusion.
Ready to Start Your Treatment Journey?
Our board-certified neurosurgeons are here to provide expert evaluation and personalized treatment plans. Schedule a consultation today to discuss your options.
Schedule ConsultationAccepted by most major insurance carriers and plans.
Many of our physicians are in-network with major insurance plans, including Aetna, Blue Cross Blue Shield, Anthem, UnitedHealthcare, Cigna, and more. Coverage can vary, so feel free to call us—we're happy to check your plan for you.
Find a Physician



Questions about degenerative disc disease treatment.
Everything you need to know about diagnosis, treatment options, and recovery.